Indiana Capitol Chronicle
February 16, 2023
By
Pharmacy Benefit Managers (PBMs) were the target of senators Wednesday as they attempt to find solutions to decrease Indiana’s elevated health care costs across a series of Senate priority bills.
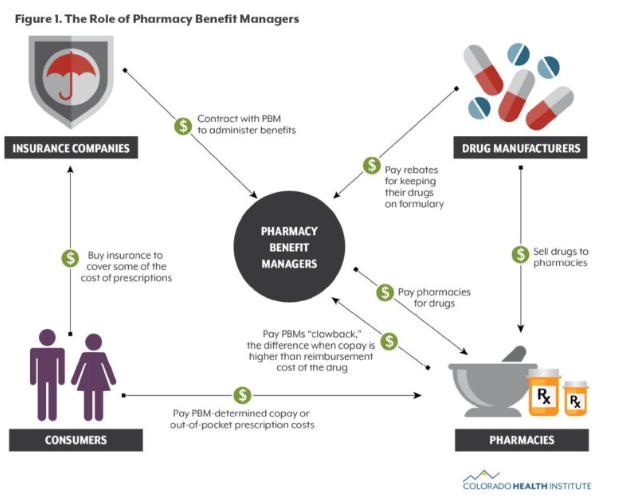
Senate Bill 8 would require the entities to pass on rebates they receive from drug manufacturers to the patients buying medications. PBMs are third-party administrators of prescription drug programs that negotiate discounts or rebates with manufacturers for their clients, usually insurers or pharmacies.
But testimony differed about why prices were so high, whether due to the PBMs or the manufacturers themselves, and who would benefit under the proposal.
Sen. Mike Crider, R-Greenfield, bemoaned that stakeholders continually point fingers at each other while Hoosiers keep footing the bill.
“It seems to me the only person that makes money in that system is everybody else except for the person that needs the drugs,” Crider said. “The person that loses at the end is the person who has hypertension or some chronic illness.”
Only one senator voted against passing the measure through the Senate health committee, though she said she wanted it to continue moving through the legislative process.
“I’m voting no to emphasize the need to make changes,” Sen. Liz Brown, R-Fort Wayne, said.
The bill moves to the full chamber for further consideration.
Eli Lilly shows support
One of Indiana’s largest and most prominent employers, drug manufacturer Eli Lilly and Company, appeared before the committee praising the bill for lowering prices for Hoosiers.
“PBMs play an important role, we’re not diminishing that,” said Ed Sagebiel, Lilly’s director of government affairs. “We’re just saying that the compensation should be tied not to the price of medicine but to the value which they provide.”
Much of the discussion centered around insulin, a substance that people with diabetes cannot live without but can be prohibitively expensive. Lilly, one of the largest insulin manufacturers, has a program that caps treatments for some at $35 but has been criticized for not lowering the cost for every patient.
Lilly and several other companies were named as defendants last month in a California lawsuit for allegedly overcharging patients for insulin.
Speaking with Sagebiel was Kristina Moorhead, with Pharmaceutical Research and Manufacturers of America. Moorhead said that research suggested premiums across health plans would increase by up to $3 under the legislation.
Neither could directly answer a question from Sen. Jean Leising, R-Oldenburg, about who would end up on the losing end of this bill’s actions. And they weren’t clear in a response to Brown about whether drug manufacturers like Lilly could make all of their products more affordable by working outside of PBMs.
Opposition to the bill
Senators spent a significant amount of time questioning the testimony of Joey Fox, a lobbyist representing CareSource as well as the Pharmaceutical Care Management Association on behalf of PBMs. CareSource is an insurance company representing roughly 74,000 Hoosiers.
“Before you today is a bill that purports to lower the cost of prescription drugs and yet somehow does so miraculously, without pharmaceutical manufacturers losing a single dollar,” he said.
Fox said that rebates from drug companies to PBMs aren’t “out of the goodness of their hearts” to lower drug prices but rather a way to secure their share of the market.
“The best way to lower the price of drugs is to lower the price of drugs. If the price of drugs weren’t so high, my clients wouldn’t have to be there to negotiate discounts,” he said.
Similar to bill proponents, Fox couldn’t directly identify winners and losers of rebate negotiations when asked by Sen. Mike Bohacek, R-Michiana Shores.
“There’s really no assurance that this is going to trickle down to either higher premiums or lower premiums in this drug space,” Bohacek said. “(Consumers) are going to get a lower price and that’s the one assurance I see in this bill.”
Lawmakers decry complex system
Congresswoman Victoria Spartz, of Indiana’s 2nd Congressional District, testified in support of the bill — an unusual move for the former state senator.

“We have significant oligopoly problems in all sectors, in every part of the market,” Spartz said. “I appreciate that you’re dealing with this issue because… the federal government is slow and not really where we need to be.”
She blamed the lack of competition and consolidation of health care entities as the cause of high prices, saying more needed to be done.
“If we don’t deal with this issue, we’re going to have a full government takeover of healthcare,” Spartz said. “I think you’re moving in the right direction.”
Crider described it as a system where manufacturers charged ten times the cost of the drug’s production and PBMs or insurers promised to decrease the price for their policyholders to only twice the real cost.
“This is magic money and it’s a shell game,” Crider said. “I don’t understand why all the people in the insurance industry and everybody else can’t figure out that my constituents are the ones that are getting shafted.”
Leising echoed Crider, saying she had some constituents who paid for drugs from Canada to get around exorbitant prices at home.
“In some ways, I just want to… do away with all of this stuff,” Leising said about the current system.
Read More on Indiana Capitol Chronicle.

